Finding Strength Within the Weakness
I’ve been mulling this one over for a couple of weeks now . . . contents include Disney, gunfire, panic, death, triumphs, Jesus, and love.
When my mom fell and broke her femur, we were finishing up our vacation in Orlando, Florida. We had already purchased tickets for the following day at Magic Kingdom. As I sat stunned, contemplating my options, after receiving the news of her injury, I was frozen in fear. How could I possibly fly out of Orlando . . . alone? The mere thought of doing so caused a surge of overwhelming anxiety to rage through my system. The trauma recovery expert in me, virtual clipboard in hand, began checking off the “how to stay calm and re-regulate your system” boxes. Meanwhile, the trauma survivor, little Teri, was curling smaller and smaller into a ball in a corner, wanting nothing more than to hide away until it was safe to come out of that protective shell again.
I elected to finish the last day and a half of our vacation then travel to Cincinnati once we returned home to Hilton Head Island. That gave me a small reprieve to get my bearings. We took off to Magic Kingdom the following morning. I’d had so much fun at the previous theme parks we’d visited earlier in the week and Kennedy Space Center a few days prior, I thought nothing of heading off to Disney for another adventure. When we pulled into the parking lot, I felt the first surges of old panic patterns start to emerge. My eyes were scanning for cover. We were being directed to a wide-open parking area, trees lining the outskirts of the lot, a monorail cutting across the horizon just ahead of us. All I could think about was running for cover, even before leaving the safe confines of our vehicle. We stopped to ask the attendant if I could be dropped off closer, but he willfully ignored my pleas from the backseat and waved us on to pull on ahead to the next available spot in row too-wide-open-for-someone-teetering-at-the-edge-of-a-PTSD-breakdown.
As we parked, the surges became too much to corral any longer. I stepped out of the vehicle and my legs stopped functioning. My brain screamed for safety. My eyes darted about seeking cover. I was back in 1988 St. Bernard, Ohio, behind a bank, scrambling from gunshots, staring down the barrel of a Luger as it beckoned my lifeforce, trying to decide between death and death as I willed my one-thousand-pound legs to move. I chose possible death over imminent death and ran, as fast as cement legs can run, back toward the gunfire, or in real world time, to our parked car. I jumped into the backseat, pulled a blanket over my head, and sobbed. I set it free. My body was trembling, my cries given voice, and I told the kids, “Just go. Just go have fun.” Then to Jen, “Please take me back to the resort. I need to go. Hurry.” As she drove me back to The Fountains, I continued to release my overwhelm, hidden under a blanket in the backseat. I then climbed into bed and did the same there. I sobbed and shook and sobbed and shook some more until my body was exhausted and relieved of that stored negative energy.
Once calm, I contemplated the events of the previous week . . . no, months . . . oh hell, two years. Moving from Ohio to South Carolina mid-pandemic, Covid isolation, mycotoxin poisoning and resulting illnesses, overwhelming debt from the mold remediation and medical expenditures (our trip to Orlando was a free week we’d been holding onto from a timeshare), numerous attorneys informing us we have a great case due to the lies on the disclosures but they won’t represent us due to “no guarantee of money payout”, my oldest son’s journey from his personal darkness into a brighter future, my youngest son’s travels from toxic servitude to dreams coming to fruition, traveling far from home via car for this trip (I’m not a highway fan!), and my mom’s fall and emergency partial hip replacement. It all came crashing down upon me in the Magic Kingdom parking lot.
We returned home the following day. Me back in the rear seat with a blanket over my head. Dissociating into Encanto on my Disney+ app as we zipped northward back into the Lowcountry. As I hugged our dogs after arriving home, feeling safe enough to discard my hermit crab shell of a blanket, the fear prickled into conscious thought again . . . hey, T, you need to get to your mom. So, how’s that gonna happen?
I had been gifted a 6-week somatic healing course by a podcast guest and it just so happened to start the week we returned from our trip. I prayerfully considered my options for returning to Cincinnati to help my mom and elected to find my way back (that was still up for consideration on HOW I’d get there) once she was out of rehab so I could help her transition from the rehabilitation facility back to independent living in her cute little retirement community. Whew! Another reprieve from traveling . . . alone.
I was continuing my weekly EMDR therapy, something I had gifted myself soon into the mycotoxin poisoning diagnosis, ensuring I was taking care of my mental health as I battled the horrific physical symptoms. I wanted to make sure I wasn’t developing food phobias after bouts of my throat closing up and emergency room visits due to food reactions (unbeknownst to me at the time, histamine intolerance from mast cell activation due to mold toxicity can result in anaphylactic reactions). Adding somatic healing to my already enormous coping skills toolbox just felt right. I had also visited the Harmonic Egg, with its sound, light, and vibration energy, and had my world rocked by the experience. As I waded into the world of somatic healing, I found myself learning new ways of sitting with anxiety symptoms as they arose. Nutrition was also brought to light and the fact that beans have a powerful part in removing adrenaline from the body. Something I had not yet learned in my research over these past 9 years of trauma recovery work.
I started adding chickpea pasta, black beans, and other bean sources to my diet. I started practicing sitting with my overwhelm as I began challenging myself. I walked further out into the open spaces of our beach then honored my body parts as they tingled with warnings. I acknowledged their messages of needing to hide or run or find that always elusive safety I’d been seeking since childhood. I gently placed my hand upon my arm as it vibrated with an adrenal surge, stating, “I feel you and acknowledge your anxiety. Let’s just be with it.” And then I’d just stay . . . stay . . . stay . . . as long as I could sit with it. My hand gently placed on whatever spot felt activated. If it moved, I would simply follow it, touch it, acknowledge it, talk to it, stay with it, thank it for its warning, then stay with it some more.
And so it went. Mondays, Wednesdays, and Fridays for that 6-week course. Me absorbing, practicing, learning, growing more than ever in my trauma knowledge. Both professionally and personally.
All the while, the deadline of my mom’s release from rehab was looming closer. I had to make a decision. I finally bought the damn plane ticket and BOOM! A kidney stone attack within hours of my flight back to Ohio. Seriously? There I was in the hospital, racking up $86K in hospital expenses from two different hospitals (sinful, isn’t it?), asking Allegiant Airlines from my hospital bed for a credit due to emergency surgery. They thankfully were beyond helpful and made a medical exception, cancelling my roundtrip ticket from SAV to CVG.
Working from a fetal position of pain from the stent the doctor placed during surgery, I was able to appeal the Medicare decision to boot my mom from rehab and win the appeal. I needed just a few more days to recover and make it the required week to get the stent removed. I was desperately avoiding the narcotics being prescribed and worried silly about the impact the antibiotics might be having on my system. The physical healing work I had done over the past year, bringing all of my labs back into normal ranges, was being threatened by western meds. I had to have faith that all was unfolding, however, as it needed to reveal whatever lesson I was needing to learn. I only took a few doses of pain medications throughout the entire ordeal. From initial emergency room intensity, through surgery, next day hospital stay, and upon returning home. Instead, I sat with the discomfort, honoring it, learning from it, allowing my body to heal. I used it as an opportunity to learn to sit with discomfort.
My stent was removed Monday morning and my flight was rescheduled for Friday morning. My anticipatory anxiety was coming in larger waves. And each time, I gently placed my hand on the spot I felt it rising, pulsating, or stirring. I sat with the discomfort. I listened. I honored. I loved. I comforted. I promised little Teri to hold her on my lap on that flight and keep her safe.
Friday morning, I had to be at the airport by 5:15 AM for a 6:45 AM flight. Funny how God works in my life at times. Our tiny little airport is never crazy busy. But that morning . . . a line out the door! Everyone in the Lowcountry must have wanted out early that day. I snaked my way through the line up to the security area, only to have my bag searched due to one of my toxin binders setting off the sensors, and then having a pat down. I hustled to the gate only to hear over the speaker, “Zone 4 is now boarding”, Yep. Zone 4 on my boarding pass. No time to sit in a seat and panic. Straight onto the jet.
I have this habit of always touching the outside of the plane upon walking through the doorway onto the flight and saying softly, “Thank you”. Thanking it for keeping me safe in flight. For taking me to my family or whatever destination I’m heading toward. I found my seat, 8C, or so I thought. An unpleasant woman advised me I was in her seat. I was on the wrong side of the aisle. I hopped over to my seat and noticed both seats next to me were empty.
A little backtrack here. I had sent up a prayer as I maneuvered my way through the security gate line, asking Jesus and Mary to be with me on the flight. I said, “Jesus, if you could sit on one side of me, and Mary if you could be on the other side, in the aisle, just holding my hand, that would be great. Thank you! I love you!”
The plane was nearly full when along came a young college-aged man, who scooted past me and sat down directly next to me. The doors were fastened shut and the flight attendant announced, “We have a sold-out flight today. All seats are full. Please be sure you are in your assigned seat.” The young man next to me hopped over to the window seat, pulled the shade down, smiled at me, and said, “I guess this is the only empty seat on the flight!” And I smiled. Knowing it wasn’t really empty. I reached my hand over and felt His presence with me. Thanks, Jesus, for being here with me.
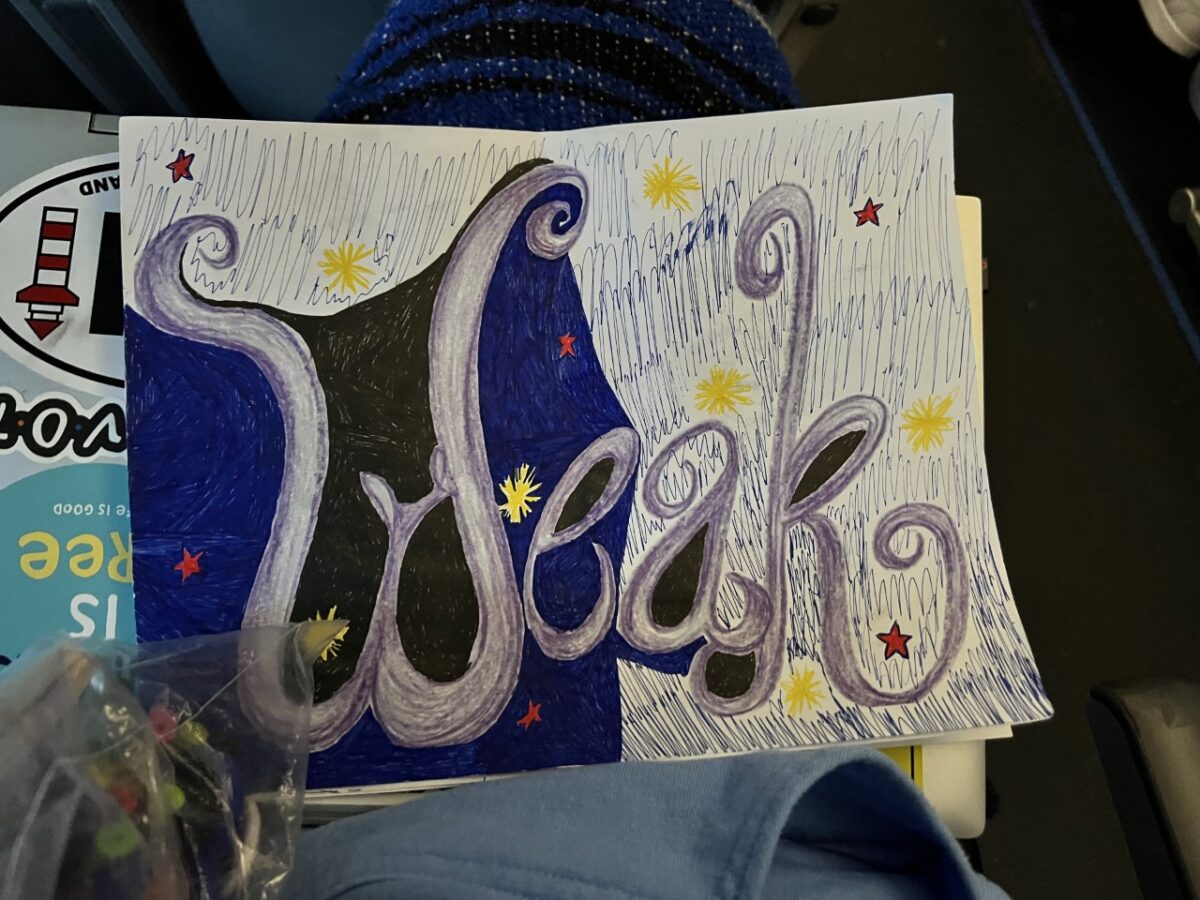
Within minutes, I felt myself being pressed into the seat as we launched down the runway, then up into the smoothest takeoff in my life. I thought perhaps we hadn’t even left the ground. No bumps or jostling as we climbed. I found my way into my bag of activities. There was my Grandma Kitty’s rainbow rosary, my favorite smooth green calming stone, 250 gel pens, a Zen coloring book, my WEAK copies (more on that in another blog), 2 fidget spinners, and my Air Pods. I popped my pods in and listened to some singing bowl music as I started coloring one of my WEAK copies with all of the black and blue pens I could find in the bag.
The first intrusive thought popped in about 20 minutes into the flight, after that first ding ding from the flight staff disrupted my coloring and song meditation, “Hey, T, you’re probably 30,000 feet in the air right now.” Woooooooosh! The adrenaline hit my right forearm. I slowed my breath purposefully. I set down my coloring materials and gently placed my left hand on my arm. I thanked it for the warning. I reminded it that angels were beneath the jet, guiding us along our path. I smiled remembering my therapist telling me she likes to envision the jet in a giant bubble just rolling along the earth. So, I went with that thought, too. Then I envisioned giant running shoes under the plane, and this big metal beast cruising along, careful not to step on houses and cars as it bound over mountainous terrain. I couldn’t help but smile. I told the thought, “I don’t have time for you right now so I’m going to place you on this shelf. I’ll get back to you later.” So, in a way, I honored it.
I decided to shift music gears and popped it on shuffle. I was now allowed to open my laptop and found Sudoku. I danced in my seat, smiling, singing along to my eclectic mix of tunes, playing Sudoku, holding my calming stone in my left hand, grateful for the radiating presence I could feel coming from that “empty” seat next to me. Mary was present but I believe she was visiting with a few other folks who may have been experiencing some overwhelm. I had put a wall of protective boundaries around me upon sitting down and noticing the bouncing legs and fidgeting happening in the people sitting nearby. I offered them all a peaceful flight and whatever calming resources they needed but asked their energy to keep at bay from my personal space. As an empath, if I don’t do so, I can be overwhelmed with others’ energy.
My ears started popping and I realized we were on our way down! Tears began to flow down my cheeks as I simply allowed them their course. I said to myself, “Teri. You’re a freaking rock star.” I sat beaming in that seat, with my laptop, calming rock, gel pens, Zen coloring book, and a big giant WEAK staring me in the face. I found my strength within my weakness. I hugged little Teri tight and whispered to her, “WE DID IT!”
I had last flown alone, traveled alone, when I was 15 years old. I flew to New York City, landing in Newark, on Christmas morning. The Empire State building had been lit up in red and green lights. My best friend had moved to New York after her parents divorced and her dad took a job in Manhattan. I was headed on a ski trip with her and her family in Killington, Vermont. This was before date rape, and a gang attack, and attempted rape by a police officer, and a stabbing, and bank robbery number one, and a gun held to my head, and bank robbery number two where that same gun murdered my coworker, and that fateful day of running with cement legs behind a bank as that Luger misfired at me.
This flight was the peak of triumph. This moment. This celebratory whisper of WE DID IT! And WE did. Thanks, again, Jesus, for sitting beside me. Figuratively and literally. That flight really was full, with no empty seats.
As a P.S. on my flight back, same announcement. The lady in the window seat looked at me as we landed at SAV and said, “How lucky were we that the only empty seat on this flight was between us?” I just smiled. Jesus did, too.
* As a side note, upon contacting Disney after returning from our trip, advising them about the lack of trauma-sensitive practices by Magic Kingdom staff, I am happy to report that their response was wonderful. They have a no-refund policy, yet we were refunded for the two tickets we did not use that day.